Achilles Tendon Rupture Rehab: From Injury to Return to Sport
What is the Achilles tendon?
The Achilles tendon is the thickest tendon in the human body. It’s located in the back of the lower leg and attaches to your calf muscles (gastrocnemius and soleus). The Achilles tendon shortens with plantar flexion (think of a dancer pointing their toes down and away from their body). The Achilles tendon lengthens with dorsiflexion (think toes being pulled up towards your nose).
Plantar Flexion
Dorsiflexion
How does an Achilles tendon tear happen?
Achilles tendon tears happen with a single high-load ankle dorsiflexion movement. There is typically an acceleration-deceleration component associated with Achilles tendon tears. This literature suggests that this is why we see Achilles tendon injuries in an active sports population such as football, tennis, and basketball players. The research demonstrates that Achilles tendon tears are usually all or none, meaning there are rarely “partial” Achilles tendon tears that occur in sport.
Mechanism of Injury
The athlete typically reports the sensation of being kicked in the back of the leg when their Achilles ruptures. They also report feeling a “pop” when the Achilles tendon tears.
Why does an Achilles tendon tear happen?
Achilles tendon tears happen for several reasons, and are most commonly seen in men between the ages of 30-50.
There is evidence that degenerative structural changes that occur over time to the Achilles tendon reduce the ability for the tendon to tolerate tensile forces. This happens when jumping/cutting athletes are overtraining and overloading their Achilles tendon with a lot of plyometrics and change of direction.
It is known that other health conditions can increase the risk for an acute Achilles tendon rupture. That includes thyroid dysfunction, diabetes, inflammatory/autoimmune disease, and more. With that said, the typical athletic population does not have these conditions.
It’s also well documented that drugs such as anabolic steroids and fluoroquinolones (antibiotics) cause a disorganization of the collagen fibrils of the Achilles tendon, which decreases tensile strength of that tendon.
Should I have surgery for an Achilles tendon tear?
If you’re an athlete or a younger, more active person, then the short answer is yes. The British Medical Journal (BMJ) published a review of the literature which found that operative treatment for Achilles ruptures reduced the risk of re-reputure compared to nonoperative treatment. It should be noted that there was not a significant number of re-ruptures in either group, but that the difference between groups was defined as “significant” by the researchers.
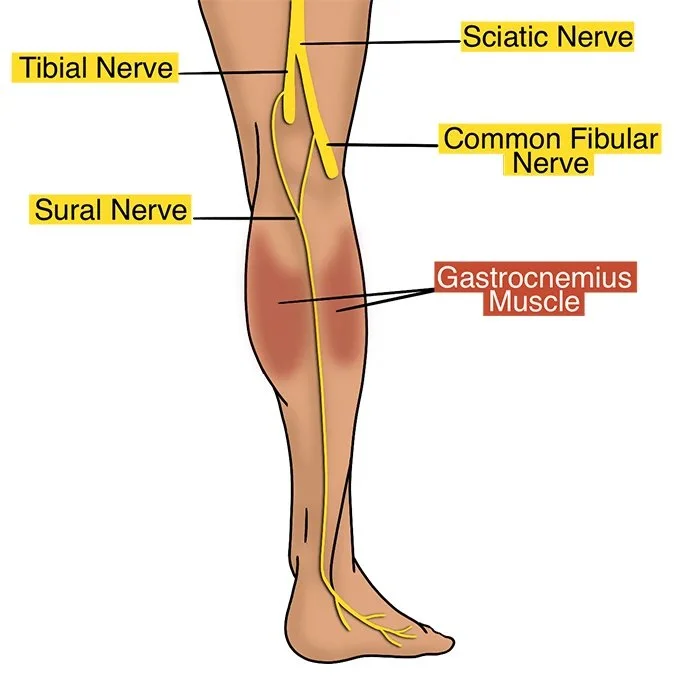
Surgery always comes with complications- that same review of the literature found that those who had surgery to repair their Achilles tendon were significantly more likely to experience complications compared to those who chose to go the nonoperative route. The complications that are most common after Achilles tendon repair are infection of the wound and damage to a sensory nerve in that area called the “sural nerve.”
Making the decision to have surgery is always a shared-decision making process between the athlete and their medical team, so be sure to have an open dialogue with your team!
Physical Therapy for Achilles Tendon Repair
Postoperatively, patients are typically in an Achilles splint to help maintain plantarflexion (to avoid any dorsiflexion and stretch of the Achilles tendon). You will use bilateral axillary crutches during this time. When the surgeon clears the patient, most patients transition into a controlled ankle motion (CAM) walker boot, still with axillary crutches. The weight bearing status will be determined by your surgeon. Wedges are placed within the boot to make sure you don’t reexpose the Achilles tendon to dorsiflexion too suddenly.
Achilles Tendon Rupture Splint - Image from Thetis Medical
Controlled Ankle Motion Walker Boot - Image from The Foot & Ankle Clinic
CAM Boot Achilles Heel Wedge - Image from Brunswick Health
Week by week, you’ll be instructed to remove layers of the wedge until you’re comfortable walking with the boot and no wedges. Your physical therapist will guide you on when your gait looks good enough to have you walk with one axillary crutch (and then with no axillary crutches).
Weight bearing precautions, types of boots, and heights of wedges are surgeon / practice specific, so we advise consulting with your surgeon about this first.
The early days after your Achilles repair may feel like you can’t do much. It’s important to remember to focus on what you can control. There are plenty of exercises that you can perform at other joints while you’re unable to safely load your foot/ankle muscles and your calf.
Below are some of the exercises we utilize with our patients in the early stages (Phase 1):
Quad sets with straight leg raise
Side lying hip abduction
Prone hip extension
Prone hamstring curls
Leg extensions
Every physical therapy practice is different, but we want our clients to load the other leg so that they don’t lose strength in the uninjured leg during this time.
Around week 4 or 5, we begin with ankle range of motion exercises (making sure not to go past neutral dorsiflexion). This includes ankle pumps, ankle circles, ankle inversion/eversion, and seated heel slides. We also start to perform foot strengthening exercises here such as foot doming, toe yoga, and seated heel raises (without weight).
Once the incision heals and there is no more risk for infection, we do scar tissue mobilization to the incision to make sure the scar heals flat. We also advise our clients to purchase vitamin E oil to perform the scar tissue mobilization on their own at home daily in between our sessions with them.
Around week 8 or so, the Achilles boot starts to come off for walking. When that happens, we don’t want our patient walking in a flat shoe. We want the shoe to have a high heel drop and we include a heel lift / wedge in the regular shoe first. Your therapist will wean you off the wedge and to a regular shoe over a period of 2-4 weeks. At this time, your therapist can also begin to mobilize the joints in your foot manually to allow for restored range of motion of the joints that have gotten stiff from being in the Achilles boot. You’ll also be instructed to perform progressively more stretching to your calf muscle (non-weight bearing calf stretching, then eventually with weight bearing calf stretches months later).
This stage of your Achilles rehab (around week 8-10) is when you’ll start to feel like you can do a bit more strengthening exercises. Your therapist will guide you on when and how, but you’ll be adding weight to your seated calf raises and you will begin to introduce bilateral standing calf raises provided you can walk in regular sneakers without wedges and without pain. Rebuilding calf strength is the most important part of Achilles tendon repair rehab. We like the chart below from this study as a reference. The researchers discuss exercise progressions that incrementally load the Achilles tendon.
Image from National Library of Medicine Article
You’ll be shown how to progressively load your calves with weight. Once you can reach at least 75% of your body weight with a double-legged calf raise, your therapist will show you an eccentric variation of a calf raise (up on 2 legs, down on the injured leg).
Double to Single Leg Calf Raise
Single Leg Calf Raise
As that is tolerated well, your therapist will show you how to progress to a single legged heel raise variation. You’ll need to progressively load the single leg heel raise with weight in preparation for a return to running. This is all initially done on a level surface to protect the injury site, but eventually you will progress to a deficit heel raise off the edge of a step. You will simultaneously be performing weighted seated calf raises, which loads the soleus muscle.
Deficit Heel Raises
You’ll also get cleared by your physical therapist to start stationary cycling (typically with the boot on, then weaned off). This will help you to start rebuilding your cardiovascular conditioning.
In these mid stages of Achilles recovery, you’ll also be working on balance, stability, and strengthening of other joints. Some of the exercises you’ll be incorporating in this mid-stage (weeks 8-12) will be:
Leg press
Planks (with Achilles boot) or injured leg off the ground
Hamstring machine curls
Here we begin to introduce more functional movement patterns to the athlete as well, such as squats, lunges, step ups and step downs, single leg leg press, etc. These are progressively loaded with weight, to tolerance.
As the calves gain strength and you develop strength and endurance, your physical therapist will introduce plyometric activities into your protocol. These usually begin with “rebounding calf raises.” This means that the speed of the calf raise is faster on the way up, but that your feet still don’t leave the ground. If that gets tolerated well, your therapist will guide you on band supported double-legged hopping, then unsupported double-legged hopping. When that goes well, your therapist will show you how to progress towards single legged hopping.
Rebounding Heel Raises
Pogo Hop Variations
Forward Pogo Hops
Return to Running After Achilles Tendon Repair
We introduce running into the patient’s training protocol somewhere around month 4-5. A return to running is based on both a time-based criteria, but also on objective data points. There is no universally accepted time to return to running in the literature, but month 4-5 is when we find clients begin to meet the criteria recommended. We want to see that you can perform single leg heel raises with at least 90% of the height of the uninjured leg. The evidence is clear that your ability to perform a single leg heel rise is an indicator of better outcomes after Achilles tendon rupture. The research also shows that heel height deficits after Achilles tendon ruptures is an indicator of ankle complications years later.
When reintroducing running, your therapist will create a “jog:walk” protocol for you to follow. It typically looks as follows:
Jog for 0.1 miles, walk for 0.1 miles (5-10 cycles) (1-2 miles total)
Jog 0.2 miles, walk for 0.1 miles (5-10 cycles) (1-2 miles total)
Jog 0.3 miles, walk 0.1 miles (5 cycles total) (2 miles)
Jog 0.4 miles, walk 0.1 miles (4 cycles) (2 miles)
Jog for 2 miles, then progressively increase by 10-20% per week until 3-4 miles
Introduce run:walk, which is more aggressive than a “jog:walk”
Your therapist will guide you through the process, as there is a ton of nuance that goes into this decision making process. We typically advise our clients to jog:walk 2-3 days per week, with at least 1-2 days in between sessions to monitor for any symptom response.
Return to Sport After Achilles Tendon Repair
Your physical therapist and surgeon will help guide you back to sport after your Achilles tendon repair. We like to see that your weighted calf raise reps are within 10-15% of the uninvolved side. We also are sure to include the following plyometric exercises as we phase you back into your sports:
Squat jumps
Double-legged forward jumps / hurdle jumps
Single-legged forward jumps / hurdle hops
Cutting drills
Sport specific change of direction drills
Jumping Plyometrics
Returning to sport is a continuum that starts with what we call “return to play.” This means you’re playing at a lower intensity, for less time than usual, and with less frequency per week. Most athletes will practice with their team in this phase for a couple months. You’ll still be working on performance-based rehab during this time. This typically occurs around 6-9 months.
The next phase is what we call “return to sport.” This is when you will return to playing in games, with load management. This means you likely won’t play in back to back games and you’ll be on a minutes restriction. This typically occurs between 9-12 months.
As long as everything goes smoothly, you’ll enter what we call “return to performance.” This is when you are approaching your previous level of performance (pre-injury status). This can take anywhere between 1-2 years.
Conclusion
Achilles tendon rupture rehab is a long journey. It’s important that you trust the team you’re working with. If you (or someone you know) are recovering after an Achilles tendon rupture and you’d like to consult us, click the button below to speak with one of our physical therapists.
Disclaimer: This is not intended to be formal medical advice. Your individual needs should be met by the appropriate health care practitioner. Please consult with a trusted provider.
Dr. Paul Nasri, PT, DPT, OCS, COMT
Doctor of Physical Therapy
Orthopedic Clinical Specialist
Certified Orthopedic Manual Therapist