Iliotibial Band Syndrome Physical Therapy
What is iliotibial band syndrome?
Iliotibial band (ITB) syndrome is a condition in which the ITB and surrounding structures become irritated at the outer knee during repetitive motions of the knee.
Patients with ITB syndrome will report lateral (outer) knee pain that is located 2-3 cm above the knee joint, although symptoms may travel up along the ITB itself. Patients with ITB syndrome often report crepitus (clicking), snapping, or a popping sensation in that area.
ITB pain results from compression of the fatty tissue between the ITB and the femur (outer thigh bone). This compression occurs as the knee bends past 30⁰, when there is maximal tension in the ITB.
For runners, compression of the ITB occurs during the first half of the stance phase of running.
Initially, runners with ITB will experience pain later on towards the end of a run, which eventually progresses to earlier in the run or even at rest.
Do I have iliotibial band syndrome?
There are a few tests we use in clinic to rule in ITB syndrome:
Noble Compression Test (provocation test) this is when there is pain on compression of the ITB over the lateral femoral epicondyle (outer knee)
Ober’s Test this test assesses for tightness in the ITB and flexibility limitations of the tensor fascia latae (TFL) muscle
Single leg squat performance test may reproduce outer knee pain once the knee starts to bend
Dynamic knee valgus may be observed (when the knee dives inward towards midline during the descent)
Why do runners get iliotibial band syndrome?
Runners typically develop iliotibial band syndrome due to training error. Most commonly, we see a sudden increase in volume and/or intensity of training. This study found that faster running results in a more narrow base of gait. It is well known, according to previous research that a more narrow base of gait results in excessive crossing over while running (which we know contributes to ITB syndrome).
Therefore, it can be concluded that sudden increases in speed may not be tolerated well by the runner, leading to excessive forces being transmitted to the outside part of the knee.
Excessive Crossover
Normal Landing
According to this study, downhill running increases load distribution to the knee joint. That type of sudden increase in loading can aggravate the knee and cause ITB syndrome. Therefore, our therapists always inquire about sudden changes in slopes/grades during your running.
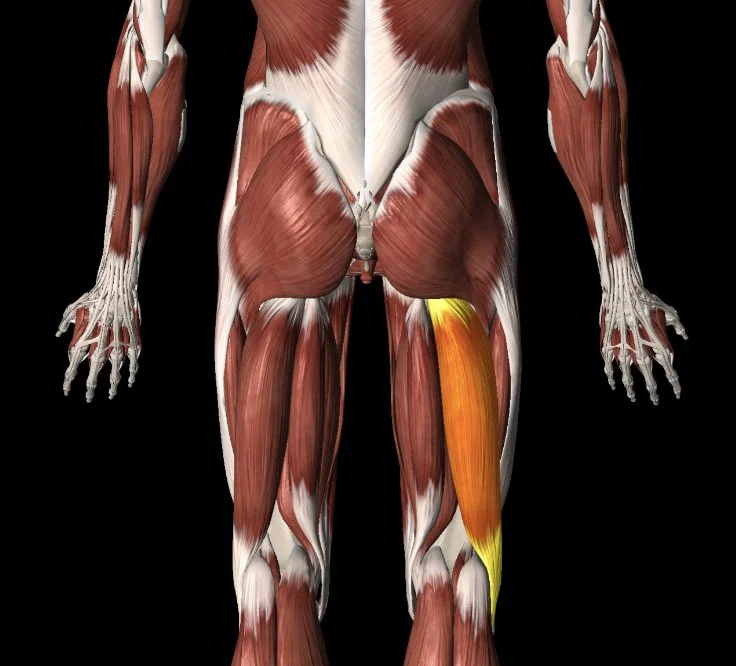
Furthermore, this study found that excessive forward trunk lean may contribute to ITB syndrome. We like to see no more than a 5-10 degree trunk lean in distance runners (that changes for track athletes, as they need to be more upright when at full speed). That same study also suggests that an excessive anterior pelvic tilt may contribute to the development of ITB syndrome. This is likely a result of the inability to recruit the posterior chain (glutes and hamstrings) when somebody is in an excessively anteriorly tilted position. If this is the case, we coach our runners to land over their center of mass by engaging the core and glutes, which will then facilitate a posterior tilting of the pelvis. This is relevant because if somebody can’t recruit their posterior chain well enough when running, they need to compensate by overutilizing their calf and hip flexor muscles to facilitate forward propulsion. The hip flexor is especially relevant here because the TFL muscle is a hip flexor that attaches to the ITB.
What are the best iliotibial band syndrome exercises?
Foam rolling the TFL, glute med, lateral quadriceps, and lateral hamstring
TFL Foam Rolling
Glute Medius Foam Rolling
Lateral Quad Foam Rolling
Lateral Hamstring Foam Rolling
Stretching the hip flexor, quadriceps, and TFL
Hip Flexor and Quadriceps Stetch
TFL Stretch
Modified side plank with clamshell
Modified Side Plank with Clam Shell
Lateral step down
(can omit the runner’s pose)
Lateral Step Down
Skater Squat
Skater Squats
Single leg RDL
Single Leg RDL
How to prevent iliotibial band syndrome
The best ways to work on ITB syndrome injury prevention is to:
Avoid training errors described above (especially early speed work and downhill running)
Have a gait running analysis performed by a running expert to determine which (if any) biomechanical variables need to be worked on. Some of the common biomechanical variables associated with ITB syndrome are listed previously in this blog.
Consider increasing your cadence by 5-10%. This research study suggests this will decrease forces transmitted to the knee and hip joint. The ITB and the muscle it’s connected to - the tensor fascia latae (TFL) cross the hip and knee joints.
Strengthen your core to attenuate forces from the hip and knee joints.
Strengthen your hip abductors, extensors and external rotators
Hip Abductor
Hip External Rotator
Hip Extensor Hamstring
Hip Extensor Glute
There is a lot of conflicting evidence on whether or not we should be stretching and foam rolling for ITB syndrome. A recent study found that a single episode of stretching and foam rolling does not affect short-term ITB stiffness. However, the researchers admit that the lack of ITB stiffness changes may be from an inadequate intervention stimulus (not enough stretching).
Anecdotally, we can tell you that we do perform foam rolling to the TFL muscle and the lateral quad muscles, but we do not advise foam rolling the ITB itself, as it can actually aggravate symptoms.
Here is a video of how to accurately find your TFL muscle and how to foam roll it. We advise foam rolling for 1-2 minutes, 2x/day.
This review suggests that long-term interventions typically include ITB stretching; however, it remains unclear to what extent stretching within a multimodal treatment actually contributes to resolving the symptoms associated with ITB syndrome. At the same time, there is no direct evidence to suggest that stretching methods have any negative effects, so we include stretching of the TFL/ITB as part of a multimodal approach to treating our patients with iliotibial band syndrome.
How do you stretch your iliotibial band? More accurately, CAN you stretch your iliotibial band?
We don’t believe you can stretch the actual iliotibial band, as it is very thick connective tissue. Our focus is on stretching of the TFL muscle. You can view a common stretching exercise that we prescribe below:
TFL STRETCH
Can I run with iliotibial band syndrome?
Iliotibial band syndrome is a soft tissue injury, so you can continue to run provided your symptoms are tolerable. We like to use a pain monitoring system in which your pain does not exceed a 4/10 during your run, directly after your run, and within a 24-hour period after your run. If your symptoms are not improving week over week, we advise that you consult with a physical therapist who specializes in running medicine.
How do you treat iliotibial band syndrome?
We begin treatment of ITBS with activity modification, allowing for running that does not aggravate symptoms. A lot of our runners ask us if they can cycle while they modify their training regimen. We don’t advise cycling, as it results in repetitive aggravation to the ITB. Consider swimming as a more suitable alternative.
If needed, ice and non-steroidal anti-inflammatory medications (NSAIDs) may help for pain relief in the short term.
Our exercises will focus on increasing flexibility of the ITB-TFL complex and hip flexor muscles, while strengthening the glutes (especially the gluteus medius).
We use movement retraining to correct dynamic knee valgus when found on the single leg squat performance test.
If symptoms persist after 8 weeks of treatment, a corticosteroid injection may be considered.
Once symptoms are less irritable, we may implement a more intensive return-to-running program for our athletes. Initially, runners should avoid running downhill or on a sloped surface to reduce strain on the ITB. If running on a track, the athlete should alternate running directions around the track to avoid only running in the same direction.
We use gait retraining for runners who run with a narrow step width / base of support. An excessively narrow stance places increased strain on the ITB. The cue here would be to increase step width. We like to tell our runners to pretend like there is a thin strip of tape between their two feet. We advise them to avoid crossing the imaginary tape.
Closing Remarks
We hope you found this article helpful. As always, consult with an expert in this field so they can advise and guide you.
If you would like to work with us to resolve your knee pain, contact us below to speak with a physical therapist.
Disclaimer: This is not intended to be formal medical advice. Your individual needs should be met by the appropriate health care practitioners. Please consult with a trusted provider.
Dr. Paul Nasri PT, DPT, OCS, COMT
Dr. Vincent Liu PT, DPT
Doctor of Physical Therapy
The Game Plan Physical Therapy